Urgent care billing plays a major role in maintaining financial stability for urgent care centers. Due to high patient volume, varied payer rules, complex coding requirements, urgent care billing requires a structured, technology-driven approach. Accurate documentation, proper coding, strong revenue cycle workflows help urgent care providers reduce claim denials, improve reimbursement timelines, maintain compliance.
What Are Urgent Care Billing Services and Why They Matter
Urgent care billing services manage the complete billing workflow from patient intake to final payment posting. These services help urgent care centers handle complex payer rules, multiple visit types, frequent coding updates.
Without structured urgent care billing services, centers face delayed payments, increased denials, revenue leakage.
Key Components of Urgent Care Billing Services
Charge capture
Accurate recording of services provided during patient visits ensures correct claim values.
Eligibility verification
Insurance verification before treatment reduces eligibility-related denials.
Coding validation
Codes are reviewed to meet payer guidelines, documentation standards.
Denial management
Denied claims are analyzed, corrected, resubmitted to recover lost revenue.
Benefits of Professional Urgent Care Billing Services
Faster reimbursement
Clean claims reduce processing delays.
Reduced denials
Accurate coding improves first-pass acceptance.
Compliance with payer rules
Billing stays aligned with Medicare, Medicaid, commercial policies.
How Urgent Care EHR Supports Accurate Billing and Coding
Urgent care EHR systems directly influence billing accuracy. Proper documentation captured during the visit supports coding quality, reimbursement success.
Improving Documentation Quality with Urgent Care EHR
Structured templates
Visit templates guide providers to document required elements.
Automated coding suggestions
EHR tools suggest appropriate codes based on documentation, reducing errors.
Integration of EHR with Billing Systems
Faster claim submission
Integrated systems eliminate manual data entry delays.
Reduced coding errors
Data consistency improves coding accuracy, claim acceptance.
Understanding Urgent Care Revenue Cycle Management
Urgent Care Revenue Cycle Management refers to managing financial processes from patient registration to payment collection. Effective Urgent Care RCM ensures consistent cash flow, operational efficiency.
Stages of Urgent Care RCM
Patient access, eligibility
Insurance verification prevents avoidable denials.
Coding, charge capture
Accurate coding reflects services provided.
Claim submission
Clean claims are submitted to payers on time.
Denial follow-up
Denied claims receive prompt resolution.
Payment posting
Payments are reconciled accurately.
Best Practices for Efficient Urgent Care RCM
Monitor AR days
Tracking accounts receivable helps identify delays.
Regular denial analysis
Patterns highlight documentation or coding issues.
Continuous coder training
Ongoing education improves compliance.
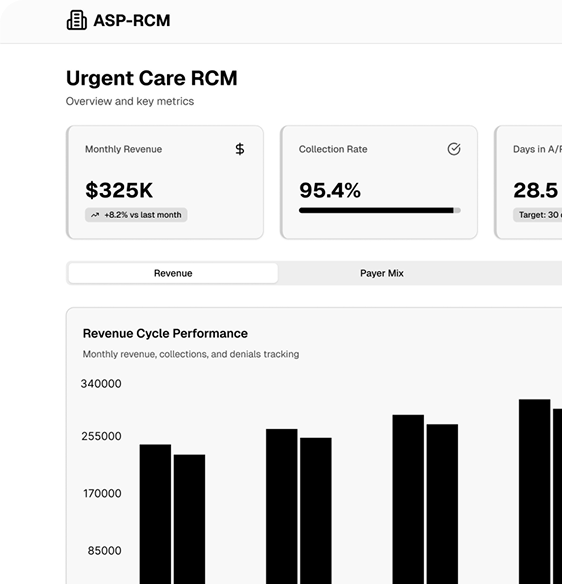
Role of Urgent Care RCM in Optimizing Revenue
Urgent Care RCM directly impacts profitability. Structured workflows reduce revenue leakage, enhance payer relationships.
How RCM Reduces Claim Rejections
Accurate CPT coding
Correct code selection minimizes payer rejections.
Proper documentation support
Complete notes justify billed services.
Monitoring Financial Performance Through RCM
Metrics, dashboards
KPIs provide visibility into revenue health.
Revenue forecasting
Trend analysis supports strategic planning.
Choosing the Right Urgent Care Billing Company
Selecting the right urgent care billing company ensures operational success. Experience, technology, compliance expertise matter.
Factors to Consider When Selecting a Billing Partner
Certified coders
AHIMA, AAPC-certified professionals ensure accuracy.
Technology integration
Compatibility with urgent care EHR improves efficiency.
Experience in urgent care
Specialty expertise reduces learning curves.
Importance of Urgent Care CPT Coding for Accurate Reimbursement
Urgent care CPT coding defines how services are billed. Proper coding reflects visit complexity, procedures performed.
Common CPT Codes in Urgent Care
E/M visits (99202–99215)
Used based on medical decision-making, time.
Wound care, injections
Procedure-specific codes improve reimbursement accuracy.
Minor procedures, splinting
Proper coding avoids underbilling.
Avoiding Denials with Accurate CPT Coding
Modifiers
Modifiers clarify special circumstances.
Documentation support
Clear clinical notes validate services.
Audit readiness
Accurate coding reduces audit risk.
Future Trends in Urgent Care Billing, RCM, and EHR
Technology continues to transform urgent care operations.
AI and Automation in Coding and Billing
AI tools identify missing charges, coding gaps, denial risks. Automation accelerates billing workflows, improves accuracy.
EHR Integration and Real-Time RCM Monitoring
Real-time dashboards provide immediate visibility into revenue performance. Integrated systems improve data flow, reduce errors.
Conclusion
Urgent care billing success depends on accurate documentation, efficient urgent care EHR usage, strong Urgent Care Revenue Cycle Management, compliant urgent care CPT coding. Professional urgent care billing services support faster reimbursement, reduced denials, financial stability. Investing in experienced billing partners, advanced technology ensures long-term growth for urgent care centers.